- Birth Control
- Bladder Issues
- Breast Care
- Menopause
- Osteoporosis
- Pap Smear
- Pelvic Pain / Endometriosis
- Pelvic Ultrasound
- Vaginal Discharge
Birth Control
Birth control can be used to regulate one’s menstrual cycle, provide symptomatic relief for certain conditions and /or prevention of pregnancy. Approximately twelve million women in the United States use birth control.

There are several different types of delivery methods:
- Oral contraceptives aka “The Pill” – There are three different options:
- Monophasic- delivers same amount of progesterone and estrogen every day. This is a better choice if having headaches because there are less fluctuations of hormones
- Biphasic- delivers the same amount of estrogen every day for the first 21 days.
- Triphasic- has constant or changing estrogen concentrations and varying progestin concentrations throughout the cycle.
- Patch – This is applied to the skin. You should change once a week for three weeks, then you get your menses on the off week. Apply a new patch a week later.
- Ring – This is a device that is inserted into the vagina. Leave ring in the vagina for 3 weeks then take out. Have your menses for one week then replace the ring.
With the pill, patch or the ring, one can use it continuously to eliminate a monthly menses altogether. For example, if you have endometriosis, heavy menses, headaches or don't want a monthly menses, you may consider this.
The pill, patch and ring contain estrogen and progestin, which prevents the ovaries from releasing an egg, changes the lining of the uterus, and changes the cervical mucus. - Shot/injection – This is a good option for women who don't want to take a pill, use a patch or the vaginal ring. The shot is given every 3 months in our office.
- Implantables and intrauterine devices (IUD like Lilleta and Paraguard). Mirena is a hormone releasing system that is implanted in your body during a visit to the office and prevents pregnancy up to 5 years.
- Tubal Ligation - is surgical procedure to prevent pregnancy. It has commonly been called "getting your tubes tied." It is also called a female sterilization. Tubal refers to the fallopian tubes. Each month, an egg is released from an ovary and travels through the fallopian tube to the uterus. Ligation means to tie off. This procedure is also associated with the reduction of the risk of ovarian cancer.
- Other – There are other birth control methods including condoms (male or female), diaphragm, cervical cap, sponge or abstinence.
How do you know the right option when it comes to birth control? It depends on several things: if one has had a baby, your lifestyle, if you have acne or certain medical conditions like PCOS or endometriosis, if your menses are heavy, if you want or don't want a monthly period, or if you prefer a generic over a brand.
Talk to your us about your options today so we can help you decide which method may be right for you.
Bladder Issues
Stress Urinary Incontinence (SUI)
Any movement that applies pressure on the bladder region can cause an involuntary leakage of urine. This can be due to weakening of the muscles that hold the urethra in place or sometimes weakness of the urethra itself (failure to maintain a seal).
Signs/symptoms:
Leaking of urine with coughing, laughing, sneezing, intercourse, activity or movement which can range in severity from occasional leakage to sudden, unpredictable episodes of leaking.
Risk Factors:
Pregnancy, childbirth, heavy lifting, menopause, obesity, chronic cough, and smoking.
Treatment:
Includes biofeedback, weight loss, smoking cessation, Kegel exercises, and/or a small surgical procedure-tension free vaginal tape (TVT) also known as a sling.
Ask yourself:
- Do you experience leaking of urine with coughing, laughing, sneezing, intercourse, activity or change of position?
- Do you have to wear pads daily?
- Do you know where all the bathrooms are at your favorite places?
- Do you limit activities or find yourself leaving these activities?
If you have answered "yes" to any of these questions and this is affecting your quality of life, talk with us today about treatment options.
Overactive Bladder (OAB)
An oversensitive bladder causes it to have spasms, leading to frequent episodes of urination along with the sensation of having to go.

Signs/symptoms:
Having to urinate every hour or several times an hour (frequency), having the feeling that you have to urinate (urgency), leaking of urine if you don't get to the bathroom fast enough (urge incontinence).
Risk Factors:
Childbirth, menopause, obesity, or decreased pelvic support. However, women in their 20's can even have this condition.
Treatment:
Includes dietary modification. Some individuals can manage this by just changing their diet by removing dietary irritants such as acids, citrus, and caffeine. Medications can help calm the bladder thus reducing the number of times one has to urinate, decreasing the feeling of urinating, and sometimes helping with leaking (if it is caused by OAB).
Recurrent Urinary Tract Infections (UTI)
Urinary tract infections can occur at any time. Recurrent infections return after antibiotic treatment.
Cause:
Bacteria reaching the bladder causing an infection.
Signs/symptoms:
Burning with urination, pressure/pain in bladder region, increased urination, feeling that one has to urinate and can only void small amounts, back pain, blood in the urine, leaking, and sometimes fever.
Risk Factors:
Decrease fluid consumption, menopause, and frequent intercourse.
Treatment:
Antibiotics, increasing fluids, and cranberry juice.
Why do some individuals have several UTI's? The infection might not have cleared up all the way, or you might not have been on the right antibiotic. Make sure you have your urine sent out for culture. This allows us to make sure you are on the right antibiotic that works for that type of bacteria. Some individuals benefit from preventative treatment. Talk with your provider about the options.
Breast Care
It is important to know your breast cancer risk and how to lower it. According to the National Institute of Health, 1 in 8 women will be diagnosed with breast cancer in their lifetime. Women are one hundred times more likely to develop breast cancer than men. Twenty percent to Thirty percent of women have a family history of breast cancer.

Some risk factors include:
Being a woman, Caucasian, advanced age (more common as we get older), family history, obesity, first pregnancy after age 35, not breastfeeding, dense breasts, menses prior to age 12, having a late menopause (greater than age 55), and exposure to estrogen.
How do you lower your risk of breast cancer?
Do self breast examinations every month, yearly mammograms, follow up on abnormal mammograms (if you are told to repeat your mammogram in 6 months), BRCA testing (testing to see if you are more at risk for hereditary breast cancer), maintaining a healthy weight, exercise, no smoking, and decrease alcohol use.
Breast cancer signs and symptoms include:
Feeling a breast lump, breast pain (may or may not be present), nipple discharge, change in size/shape or feel of your breast.
We offer clinical breast exams, teaching of self-breast exams, BRCA testing, and yearly mammogram orders. If you feel something that is not "normal" call right away.
For further information about Breast Cancer log onto:
Menopause
Is Menopause Impacting Your Life?
During the menopause transition, many women experience symptoms that can affect their quality of life such as hot flashes, mood swings, trouble sleeping, night sweats, vaginal dryness and discomfort, pain with intercourse, lack of sexual desire, and urinary issues-loss of bladder control (leaking) or increased frequency (number of times one urinates), and increased risk of urinary tract infections. These symptoms occur due to the decreasing and fluctuating estrogen levels. The average age of menopause is fifty-two.
Menopause also can put a woman at risk for developing osteoporosis (ask about our in-office DEXA scan machine) and cardiovascular disease. It is important to be up to date on annual blood work and screenings (our office can set you up for these).

Vulvovaginal Atrophy, or "vaginal dryness" is a common condition that can occur during this time. The symptoms can include discomfort, burning, increased urinary frequency or the feeling that you must urinate (urgency), frequent urinary tract infections, itching, dryness, irritation and pain with intercourse.
It is a common condition and can be very much treatable, however; only a small portion of women seek treatment. Many times, it can affect a woman’s quality of life. Many women feel that they need to just deal with these symptoms and that it is part of menopause, so they just endure it. There is treatment!!!
Treatment options include:
Hormonal (small dose of vaginal estrogen) and nonhormonal (lubricants, vaginal moisturizers, etc.) Many women are reluctant to seek medical care for these issues. You are not alone. Why live with these symptoms if you don't have too. Talk with your healthcare provider about the symptoms that you are experiencing today.
Osteoporosis
Osteoporosis is referred to as "porous bones", also called the silent disease. Many times, there are no symptoms until one develops a fracture due to the bones being brittle and weak. The best way to measure your bone health is with a bone density test (also known as DEXA).
Signs and symptoms can include:
Back pain, loss of height, bent over posture, and fracture.
The exact cause is unknown; however, your bones constantly break down and new bone forms. When there is more bone breakdown then new bone being made, this causes osteopenia (which happens before osteoporosis).
Risk Factors include:
Age, family history, menopause, certain medications (steroids, acid blocking, antidepressants, seizure), smoking, decreased consumption of calcium and vitamin D, and sedentary lifestyle.
Treatments:
- Weight bearing exercises daily
- Vitamin D and calcium supplements (total of 1200mg a day of calcium in divided doses and 800-1000 IU of vitamin D a day). Do you know your vitamin D level?
- Routine vitamin D levels (measured by bloodwork)
- Medications slow bone loss, maintain bone mass and even increase bone density. Examples of these medications include Fosamax, Boniva, Actonel and Reclast.
- There are different treatment options depending on if you have osteopenia versus osteoporosis. Talk with your provider today about your DEXA (which we do in our office), vitamin D level and treatment options.
Pap Smear
A pap smear is a screening tool used in gynecology to detect abnormal cervical cells. Regular pap smears are the best thing you can do to prevent cervical cancer. Pap smears are recommended annually for women of any age that are sexually active. Women that are not sexually active should begin seeing their gynecologist by age 18 to determine if a pap smear is needed.
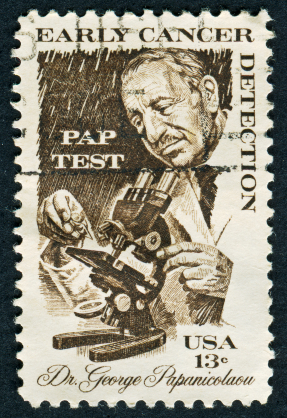
During a pap smear a speculum is inserted into the vagina helping to see the cervix. A brush is used to collect cervical cells. The cells are then preserved in a liquid-based pap and sent to a local lab to be processed. The cells are then examined under a microscope and can detect infections, abnormal cells, and cervical cancer.
An abnormal pap smear does not mean that you have cervical cancer. Abnormal cells are most likely caused by the HPV virus. Most strains of the virus will clear on their own without any intervention but do need to be monitored to be sure they are not getting more aggressive. By having your pap smear regularly, we are able to detect abnormal cells and monitor the patient by either repeating the pap smear at three-to-six-month intervals until the cells return to normal or recommending further testing.
Women who have had a hysterectomy should continue to see their gynecologist on a regular, annual basis. Depending on the type of hysterectomy performed, a pap will still need to be collected. Pelvic exams should be performed annually to rule out any abnormalities that may arise.
For two days prior to your pap smear you should avoid having intercourse. Women should discontinue use of any vaginal creams, suppositories, or medications. Lubricants should be avoided. Discontinue use of vaginal deodorants or powders. If you are having your menses you should call to reschedule your pap smear.
Pelvic Pain / Endometriosis
Pelvic Pain that is in the lower abdomen area, the area below your belly button, is referred to as pelvic pain.

Symptoms can vary and can be:
- Pain-ache, sharp, cramping, pressure, stabbing, dull, burning, comes and goes or stays and can worsen.
- You may experience this pain during intercourse, with a bowel movement, with or without activity.
Some causes include:
- Endometriosis - a condition in which tissue from the uterus (uterine lining) grows outside the uterus
- Ovarian cyst - collection of fluid in or on the ovary
- Irritable bowel syndrome (IBS) can cause symptoms including constipation, bloating, and diarrhea
- Muscular - tension or spasms in the muscles inside the vagina-pelvic floor
- Pelvic inflammatory disease - an infection that is left untreated
- Pelvic congestion syndrome - veins around your uterus and ovary become engorged with blood
- Fibroids - benign uterine growths
- Adhesions - scar tissue
- Interstitial cystitis - also called painful bladder syndrome-chronic inflammation of the bladder, symptoms of a UTI without the bacteria
- Infection - bacterial, yeast, STD
- Psychological factors - depression, chronic stress, history of abuse
- Vestibulitis - inflammation of the glands inside the vagina-pain/pressure vaginal opening
- Vaginal atrophy - atrophic vaginitis decrease in estrogen inside the vagina, associated with menopause
- Cycle related - pain prior to or during menses
- Urinary tract infection - bladder infection
Your provider will start with an exam, order an ultrasound, urinalysis, and or obtain cultures. Sometimes other imaging studies are ordered such as a CT scan or MRI. Laparoscopy, a surgical procedure, is sometimes needed to diagnose and treat the cause of pelvic pain.
Treatment depends on the underlying cause and may include pain relievers, hormone treatments, antibiotics, antidepressants, physical therapy, lifestyle modifications-diet and in some cases surgery.
Pelvic Ultrasound
Pelvic ultrasound is performed two different ways.
- The first, called transabdominal ultrasound, is performed with a transducer that is moved across the belly.
- The second, called transvaginal ultrasound, is performed with a transducer that gets inserted vaginally. Both are highly effective ways to image the pelvic organs.

During a pelvic ultrasound, images of the ovaries, uterus, endometrium, and sometimes the bladder are taken and saved to accompany the findings report. There is often the misunderstanding that ultrasound can identify organs like the fallopian tubes, or afflictions like endometriosis and adhesions. Ultrasound is not sensitive enough to image these things. Sometimes pathology of the fallopian tubes or presentation of endometriosis in an ovarian cyst is visible, but generally these things are not seen during a pelvic ultrasound. They are usually surgically diagnosed. What we can image with a pelvic ultrasound are fibroids, ovarian cysts, thickened endometrium (and sometimes polyps), and of course, normal appearing organs.
How Do I Prepare for a Pelvic Ultrasound?
For a transabdominal pelvic ultrasound, a full bladder is required. The full bladder gives a great window for seeing the pelvic organs and can also help to push bowel out of the way. It is recommended you drink 32 ounces of water one hour prior to your ultrasound. Do not empty the bladder; you will be allowed to do so as soon as your ultrasound is done.
Sometimes the bladder is not full enough to image everything, or even with a full bladder, situations arise where a transvaginal ultrasound is more appropriate. There are also times where a transvaginal ultrasound is preferable to a transabdominal one for the fact that it allows a more clear and close-up view of certain things. Instances of this would be IUD surveillance (to check for correct placement of an IUD), to image the endometrium very well (in instances of post-menopausal or other irregular bleeding), or for fertility drug monitoring (to measure growth of follicles, etc). In these cases, and some others which your doctor will tell you, it is not necessary to have a full bladder. For a transvaginal ultrasound, it’s actually best to have a very empty bladder, and often you will be asked to empty your bladder prior to your ultrasound.
Vaginal Discharge
Vaginal discharge is usually normal. However, if you are experiencing pain, painful intercourse, odor, itching, irritation, bleeding, or change in color or consistency you may have an infection.

Vaginal discharge is a combination of fluid and cells. The function is to clean and protect the vagina from infections. Color and Consistency of vaginal fluid may change and vary. Usually, the color is clear to white. If it is yellow or green, you may have an infection. Discharge may increase because of hormonal changes that correspond with your reproductive cycle.
Most common causes:
- Bacterial: Bacterial Vaginosis, Group B strep
- Sexually Transmitted Disease-STD
- Yeast
A decrease in vaginal discharge on the other hand may be the result of menopause, or hormonal fluctuations. Sometimes individuals have recurrent infection, an infection that doesn't clear up, or comes back. It is important to have cultures done to check for infection because sometimes the wrong infection is being treated. You may think it is a yeast infection, for example, and it might be a bacterial infection. Not all bacterial infections are treated with the same medication. Treatment depends on the type of infection. If you are concerned, you should schedule a visit.

